Mary Madison, RN, RAC-CT, CDP
Clinical Consultant – Briggs Healthcare

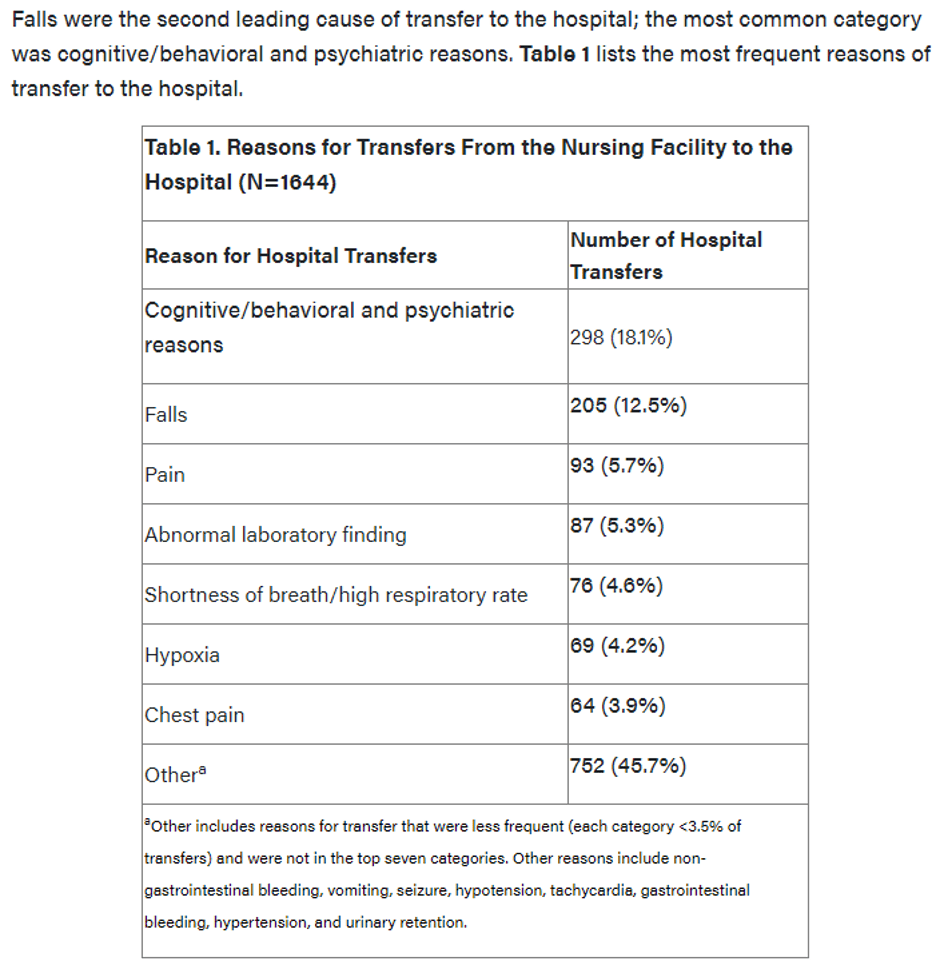
The title of this blog is the opening statement in the Description of Fall-Related Transfers in the Nursing Facility: Findings From the OPTIMISTIC Project abstract published in the Annals of Long-Term Care.
The Abstract continues with:
“Using data from the Minimum Data Set (MDS) 3.0 and the database of the Optimizing Patient Transfers, Impacting Medical Quality, and Improving Symptoms: Transforming Institutional Care (OPTIMISTIC) demonstration project, our study team compared characteristics of LTC residents transferred to hospital settings for falls with residents transferred for other clinical reasons over 27 months. Our analysis showed that history of falls, cognitive impairment, female sex, White race, and being aged 80 years or older are all significantly predictive of fall-related transfers vs non-fall–related transfers. The majority of those transferred only needed care in the ED. Our study underscores the need for continued work to identify residents at high risk for injurious falls and hospital transfers to better inform risk stratification and interventions in the nursing facility setting.”
The Introduction reports:
“Of the 1.6 million residents in US nursing facilities, about half of them fall every year, and 1 in every 3 residents falls multiple times in a year. Factors predisposing older adults to falls can be divided into three categories: extrinsic, anticipated intrinsic, and unanticipated intrinsic. Extrinsic factors relate to the environmental causes of falls and are usually considered accidental. Physiologic or intrinsic causes can be either anticipated (such as certain medications) and unanticipated (such as sudden stroke).Among older adults, those in nursing facilities fall more frequently than those residing in the community.
In a retrospective study that compared cases of falling in nursing facilities and their estimated costs, residents who fell were more likely to suffer fractures and hospitalizations than those who did not fall; in addition, falls in LTC settings are associated with higher total health care cost.”
There are 2 additional Tables in this publication that provide additional information.
I strongly recommend that all LTC facilities review and discuss this information. Identification of where your facility “falls” within the 3 categories of predisposing factors would certainly be worth your time as would a specific and continued program of reducing falls in your facility. Tables 2 and 3 will help you with such identification as a starting point for your team. Consider the last statement in the 1st paragraph of the Introduction: “Among older adults, those in nursing facilities fall more frequently than those residing in the community.”
