Mary Madison, RN, RAC-CT, CDP
Clinical Consultant – Briggs Healthcare
The OIG (Office of Inspector General) posted this 19-page report with the same title as this blog on March 15, 2022.
(OIG) based this analysis on Medicare fee-for-service claims data and Medicare Advantage encounter data from March 1, 2020, to February 28, 2021, and from the prior year, March 1, 2019, to February 29, 2020. (OIG) used these data to determine the total number of services used via telehealth and in person, as well as the types of services used. (OIG) also compared the number of services used via telehealth and in-person during the first year of the pandemic to those used in the prior year.
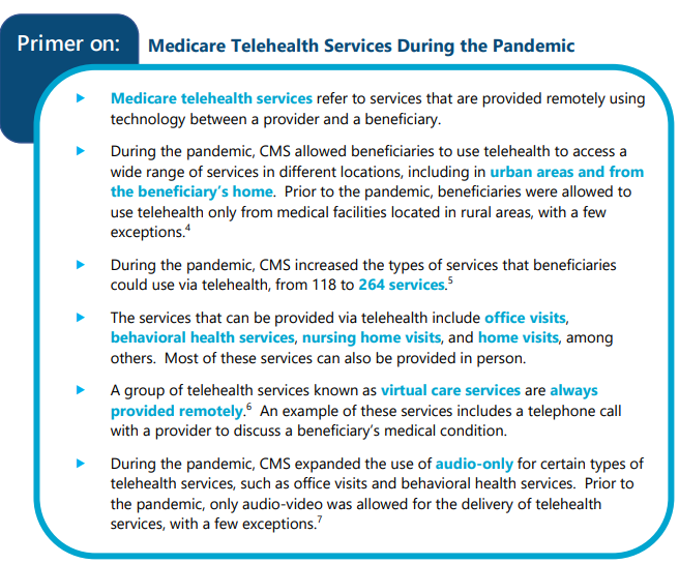
Over 28 million Medicare beneficiaries used telehealth during the first year of the pandemic. This was more than 2 in 5 Medicare beneficiaries. In total, beneficiaries used 88 times more telehealth services during the first year of the pandemic than they used in the prior year. Beneficiaries’ use of telehealth peaked in April 2020 and remained high through early 2021. Overall, beneficiaries used telehealth to receive 12 percent of their services during the first year of the pandemic. Beneficiaries most commonly used telehealth for office visits, which accounted for just under half of all telehealth services used during the first year of the pandemic. However, beneficiaries’ use of telehealth for behavioral health services stands out. Beneficiaries used telehealth for a larger share of their behavioral health services compared to their use of telehealth for other services. Specifically, beneficiaries used telehealth for 43 percent of behavioral health services, whereas they used telehealth for 13 percent of office visits.
Telehealth was critical for providing services to Medicare beneficiaries during the first year of the pandemic. Beneficiaries’ use of telehealth during the pandemic also demonstrates the long-term potential of telehealth to increase access to health care for beneficiaries. Further, it shows that beneficiaries particularly benefited from the ability to use telehealth for certain services, such as behavioral health services. These findings are important for CMS, Congress, and other stakeholders to take into account as they consider making changes to telehealth in Medicare. For example, CMS could use these findings to inform changes to the services that are allowed via telehealth on a permanent basis.
This is an extremely interesting report. Please review/share it with your team and colleagues. Did your facility/agency use telehealth the past 2+ years of the pandemic (which isn’t over yet)?
